Ketamine is a drug that seems to have a variety of uses, from inducing anesthesia in patients undergoing surgery, to inducing mind-altering states in partygoers, to treating severe depression and chronic pain. How can one drug be so multifaceted?
The answer relates to dosage and the complex ways that ketamine affects the brain, which scientists are only beginning to fully understand. Ketamine affects a wide range of brain receptors, spanning the glutamate, GABA, opioid, acetylcholine, dopamine, serotonin, and adenosine systems. That said, it seems that its effects on the neurotransmitters glutamate and GABA might be most important for its antidepressant effects.
Glutamate is the primary excitatory neurotransmitter of the brain, which means it’s the main brain chemical that’s responsible for making brain cells (neurons) activate. In contrast, GABA – its sister neurotransmitter – is the primary inhibitory neurotransmitter of the brain, which makes neurons less likely to activate. The balance between these two neurotransmitters is what controls the difference between overwhelm and calmness, stimulation and depression, and alertness and sleep. Glutamate also plays an essential role in regulating neuroplasticity, which refers to the brain’s ability to rewire itself to facilitate learning, memory, and recovery from injury.
At the doses administered in ketamine-assisted psychotherapy, ketamine induces a huge surge of glutamate in the prefrontal cortex (PFC)¹. You may have heard of the PFC: it’s the region of the brain involved in various aspects of our conscious thinking, including planning, problem solving, and attention. Ketamine basically overloads this part of the brain with glutamate-induced activity by blocking the activity of GABA neurons which are usually inhibiting glutamate release.
To understand why this surge of PFC activity can be therapeutic, we need to understand a bit about depression in the brain. Scientists have identified that depressed individuals, largely as a result of chronic stress associated with this disorder, show reduced neuroplasticity in their brains². Studies have also shown that the middle part of the PFC in particular (the ‘medial’ PFC) exhibits a loss of neuron connections and dysfunctional activity in depression³⁴. Depression-related disruptions in the PFC may relate to not being able to think clearly and to getting stuck in repetitive, negative thought loops: the hallmark of depression that scientists refer to as ‘rumination’⁵ ⁶.
By blasting the PFC of depressed patients with activity, ketamine both temporarily restores proper functioning to this region and also boosts neuroplasticity², effectively countering the two disruptions caused by depression. So, in addition to inducing a dream-like and potentially personally meaningful altered state of consciousness, ketamine induces very physical changes in your brain that pull you out of your depression – at least temporarily. Why these effects are temporary and how we can prolong the effects are topics of intense research, and to be discussed in a future blog post.
Click here to learn more about EntheoMed’s Ketamine Assisted Therapy Suite, including more details about our approach, the experience, and a form to book your first appointment.
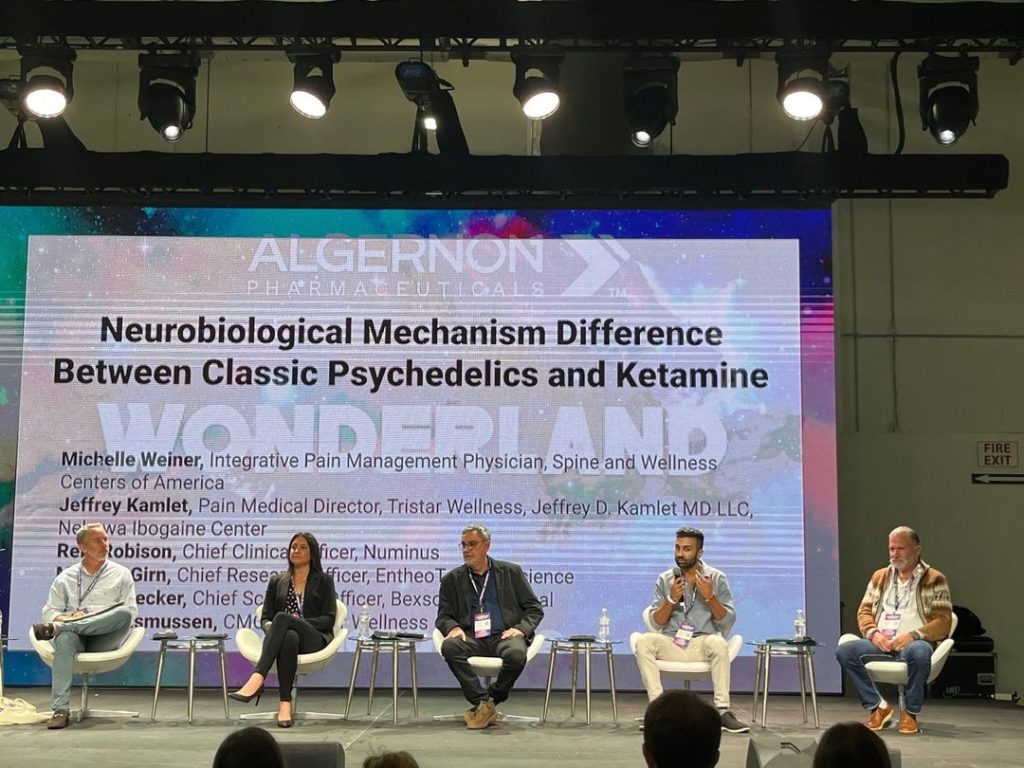
Written by Manesh Girn for EntheoTech
REFERENCES
(1) Neurobiology of the Rapid-Acting Antidepressant Effects of Ketamine: Impact and Opportunities
(2) Neuroplasticity in cognitive and psychological mechanisms of depression: an integrative model
(3) Sustained rescue of prefrontal circuit dysfunction by antidepressant-induced spine formation